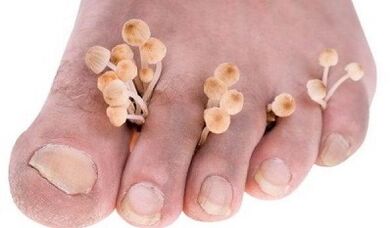
The fungus between the toes is a disease that is very easy to take.But getting rid of it is not so easy.The disease can last for years, often a bacterial infection joins it.When the first symptoms occur, it is very important to contact a dermatologist, not to self -assess.
Why the fungus develops between the toes
The fungi between the toes are the most common type of fungal infection that occurs in 70% of the population of our planet.This disease is especially common among people who are constantly in a wet or hot environment, often sweaty due to high physical activity.These include banners, swimmers, hot workshops, etc.Children are much more sick (no more than 4%), but the frequency increases dramatically in adolescence.
The disease is caused by various types of dermatophilic mushrooms: red trichopitone, interdaltsev trichophyton and some types of epidermophitons.All these pathogens are highly survived in the environment.They can last for a long time the floors in the bathroom and sauna, bathroom equipment, underwear, in shoes.
You can get infected in a bath, sauna, pool, less frequently on the beach.That is why it is so important to follow the hygiene rules: use only an individual towel, do not go barefoot in public, using separate shoes for it.
Once on the surface of the body, mushrooms produce enzymes (keratinase), which decompose keratin - the protein of the superficial skin layers.This allows the infection to penetrate the epidermis and multiply there.Mushroom membranes contain substances (manners) that can inhibit local immunity.Manin also suppress the reproduction of the surface cells of the epidermis, which is why their disposition and purification are disrupted, which as a result leads to a prolonged and chronic course of the disease.
Factors contributing to the spread and application of fungi
Such factors include:
- shoes that squeeze the legs that disturb blood circulation and do not pass air;
- playing sports and heavy physical labor;
- leg trauma with skin disorders;
- Impaired immunity, for example, against the background of diabetes, prolonged administration of certain drugs (glucocorticoid hormones), HIV infection;
- Disruption of the circulation at the legs of the legs against the background of atherosclerosis of the lower limbs, flat legs, etc.
If a person has a normal common and local immunity, the fungus will not be able to overcome the protective barrier of the skin and penetrate the skin.All factors suppressing skin immunity allow the introduction of pathogenic fungi into the epidermis without obstacles, causing a pathological process.
Symptoms of infection
When introducing pathogenic fungi into the skin, mainly areas with thin and delicate skin are influenced by interdigital gaps.This is where the infection begins, which can then spread to the whole leg.The first thing that the infected person experiences is itching and burning between the toes.
Itching can be very strong or can be insignificant or even completely absent and only appear against the background of sweating of the legs or reducing immunity.Significant itching, dryness, painful cracks in the interdigital spaces contribute to the addition of bacterial infection and the development of purulent processes.
Sometimes sluggish bubbles appear between the fingers, filled with transparent fluid, which quickly opens, forming erosion.And this type of disease can be complicated by adding a bacterial infection.
The most characteristic of the hidden course of fungi between the toes, which is characterized by periodic itching.Often, such patients do not suspect the presence of infection and spread it among others.
How does the disease flow
The fungus can be manifested in different ways.The following forms of the disease are distinguished:

- Intrigued- the most common;It manifests itself in the form of itching and burning between the toes, dryness, cracks with the release of the bite and the subsequent development of maceration (loosening the skin under the influence of the fluid);Inflammation often goes to the plantar surface of the legs and almost never at the back;Bacterial infection often joins;
- Graph- with the appearance between the fingers of the stops of the sluggish, cracked bubbles, the formation of erosion, the introduction of bacterial pathogens and the development of the pathological process according to the type of eczema spread to the whole leg, leg and even the body;
- deleted- flows unnoticed;Sometimes a slight itching occurs;A moderately thin peeling (most often between 1 and 2 or 5), very small, unnoticed by patients with cracks, appears between the toes.
The fungi in the interdigital gaps can occur as an independent disease or is a manifestation of a common infection.Often the fungi move to the nails with the development of onychomycosis.Sometimes there is a combined lesion of the skin of the feet and skin in the area of large folds on the body as well as the hands.In the latter case, the infection often develops on the principle of "two legs - one brush".
How to identify an infection
The diagnosis is made on the basis of a dermatologist examination and confirmed by laboratory tests:
- The microscopy method- under the microscope, the skin elements (rocks) taken from the lesion are examined;This is the most common method, it allows you to identify a fungal infection but cannot determine the type of fungi;
- Microbiological examination- sowing of biological materials taken from the lesion to food environments;Ground mushrooms are easy to identify, but they do not always give laboratory growth, so it often remains to focus only on the microscopy method.
The basic principles of treatment
Antifungal drugs are used to treat the fungus of interdigital gaps.If the disease does not last long, it does not progress, then external funds are used.In severe fungal infections with a tendency to spread or develop microbial eczema, antifungal drugs with general (systemic) action are used.
External use of antifungal agents requires preliminary preparation.Pathologically altered skin elements are removed from the surface of the skin: peeling, destruction of places and the remains of cracked bubbles.They try to relieve inflammation and swelling of the tissues if possible.
Conduct the following procedures:
- If there is pronounced inflammation and tissue swelling, the lotions are prescribed with 2% solutions of boric acid, special ointments;If it does not help, corticosteroid ointments are prescribed in short courses;
- In the presence of flakes and bark, the affected areas of the body surface are lubricated twice a day with salicylic oil jelly and then bath baths with 2% soda solution are made.
Only after cleaning is the basic treatment is performed.If there is a suspected mixed fungal-bacterial infection, combined ointments are used, which include antifungal, antibacterial and anti-allergic components.
Drug therapy
The most modern drugs for the treatment of such diseases are medicines, the active action of whose substance is terbinafine, which is part of the products of external use, produced by various pharmaceutical companies under their commercial names.These are 1% creams, gels, sprays and solutions for outdoor use.
This substance easily enters the epidermis.Already 4 hours after its concentration, its concentration is sufficient to suppress the vital activity of the infection.The concentration of the product accumulates in the skin gradually and after therapy is many times higher than the concentration causing the death of the fungi.In addition, it does not penetrate the middle and deep layer of the skin and has no systemic effect on the body.The characteristic of the antifungal agent is that it has an antibacterial effect, suppressing the vital activity of most pathogenic bacteria.Therefore, for the treatment of fungal-bacterial infection, additional antibacterial therapy is not always required.
The cream, spray and gel are applied to pathologically changed areas of the legs every day for 7 days.This is usually enough to completely go through all the symptoms of infection.If necessary, the dermatologist may prolong the course of treatment.
With the ineffectiveness of external treatment and common, often recurrent forms of the disease, antifungal drugs with common effects are prescribed.
With the development of microbial eczema, complex treatment is prescribed, which includes antifungal drugs, antibiotics and desensitizing agents that reduce allergic mood, inflammation and tissue swelling.In severe allergic and inflammatory processes, glucocorticoid hormones are included in complex treatment.
Folk remedies against interdalendical fungi
Folk remedies can also be effective if used properly.Traditional medicine recommends that before starting antifungal treatment, the preparatory treatment for the cleansing of pathologically altered areas of the surface of the legs.Cleaning is done in the same way as before treatment with medication.Fixed assets are then used to suppress the vital functions of mushrooms.
- Method 1.Twice a day, for 2 to 3 weeks, make the feet for the feet with infusion of celandine from a large (third of a glass of crushed grass per liter of boiling water) and then lubricate the dried surface of the feet with a 10% propolis tincture.
- Method 2.Add 20 ml of ammonia to a glass of water, moisten the bandage, wrap your toes first, then the whole leg (do not tighten!) And leave until dry;The duration of treatment is 14 days.
- Method 3.Foot baths with vinegar (for 2 liters of water - 100 ml of trap vinegar).They are held daily before bedtime for 14 days.After the procedure, dry your feet and gently sprinkle them with boric acid.
- Method 4.Required bathrooms with a touched shafts (20 g of 1L boiling water fly, insist 3 - 4 hours in a thermos).Do every day before going to bed for four weeks.After the procedure, the legs should dry themselves.Wash your feet in the morning with water.
- Method 5.Wash your feet with home soap, washing thoroughly between your fingers.Dry your legs and spread the skin with sealandine juice.Do this every day for 14 days.
- Method 6.Daily leg legs with 2% soda solution.After the bathroom, dry your feet with a well for a towel and grease with garlic oil.Wash them with soap in the morning.Garlic oil: Mix a teaspoon of crushed garlic from 100 g of oil until a homogeneous mass is obtained.
- Method 7.Take the same amount of apple cider vinegar and freshly squeezed carrot juice.Apply the resulting mixture to the affected areas of the skin of the feet several times a day for a month.
How to warn the infection
To prevent the disease, you must:
- Wear rubber shale in a bath, sauna, pool, on the beach;
- Never wear one's shoes, do not use someone's cloth and bathroom accessories;
- In the warm season, wear shoes or sandals made of light natural materials that pass air and absorb moisture;
- To conduct a pedicure, use only individual or one -time instruments.
In order to prevent re -infection, it must be:
- Treat the inner surface of shoes with disinfectant solutions, for example, formalin solutions or is the essence of vinegar;Two days after such treatment, the death of all infectious pathogens occurs.
The fungi between the toes are good to succumb to therapy with modern antifungal agents and folk methods.But it is very important to make every effort so that there is no re -infection, including through your own shoes and other personal use items.















